Introduction:
Coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been a major challenge worldwide. Data reporting manifestations of COVID-19 in pediatric cancer patients are limited. This report describes the presentation and initial management challenges of a newly diagnosed child with acute lymphoblastic leukemia (ALL) with positive (+) SARS-CoV-2 complicated by multisystem inflammatory syndrome in children (MIS-C).
Case Description:
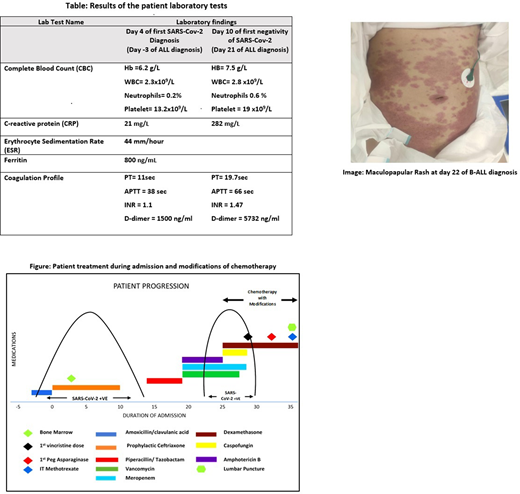
A previously healthy 9-year-old female had (+)SARS-CoV-2 following a 4-day history of fatigability. This was followed by a day of severe gastroenteritis (GE) necessitating a visit to Jaber Al-Ahamed Hospital (JAH), the designated COVID-19 pandemic center. Examination revealed hypovolemic shock, hepatosplenomegaly (HSM) and cervical lymphadenopathy. Patient also had significant pancytopenia and high inflammatory markers (Table).Bone marrow aspiration (BMA) - done 7 days from diagnosis of SARS-CoV-2 - was consistent with B-ALL. Transfer to National Bank of Kuwait Children's Hospital (NBKCH) - the pediatric cancer center - was delayed for 11 days given her (+)SARS-CoV-2, but once tested negative, transfer was complete. Due to logistical issues, lumbar puncture and repeat BM were delayed. She then developed new fever, abdominal pain and vomiting. Her febrile neutropenia (FN) was managed according to local protocol including antifungal therapy for prolonged FN. Five days into her FN, she developed hematemesis and septic shock. In addition to pancytopenia, she also had disseminated intravascular coagulation with further raise in CRP (Table). She also had a new maculopapular rash (Image). Infectious work-up was negative except for (+)SARS-CoV-2 (after 10 days of negativity), fulfilling criteria of MIS-C. Patient was transferred back to JAH according to local pandemic protocol. Induction chemotherapy as perUK-MRC-ALL 2011 regimen Afor standard risk ALL - with modifications given her MIS-C - was started after 22 days (Figure). On day 5 of chemotherapy, patient was clinically stable with negative SARS-CoV-2, therefore transferred back to NBKCH for continuation of leukemia management.
Discussion:
Although children tend to have a milder course of COVID-19, this case described a fulminant presentation initially with GE, hypovolemic shock and complicated by MIS-C, lacking any respiratory symptoms throughout her course. Until more data reporting manifestations of SARS-CoV-2 in pediatric cancer patients are available, physicians should keep high index of suspicion for leukemia in presence of pancytopenia and HSM in spite of (+)SARS-CoV-2. Prompt diagnosis of ALL is fundamental to avoid delays in treatment and consequent effects on prognosis. Logistical issues such as lack of optimum COVID-19 isolation measures in our cancer center and paucity of blood products have led to delayed initiation of chemotherapy. These cancer-related challenges have been well described.
Another interesting aspect of our case is the seroconversion to (+)SARS-CoV-2 after proved negativity. It is possible that protective antibodies were not well developed as she is immunocompromised, making such patients prone to recurrent SARS-CoV-2 infection. The re-emergence of SARS-CoV-2 has led to the diagnosis of MIS-C after fulfilling other criteria. This phenomenon of negative to (+)SARS-CoV-2 seroconversion has been reported in 20-40% of MIS-C cases.
Increased risk of venous thromboembolism (VTE) is linked to the hyperinflammatory state of COVID-19. Chemotherapy is also identified as an independent risk factor for VTE in malignancy. To avoid the collateral effects of these factors, modifications of the planned chemotherapy were implemented in our case to minimize the VTE risk. The high steroid dose with chemotherapy was also planned as a treatment for MIS-C, which is consistent with different modalities of MIS-C treatment offered in literature.
Conclusion:
Children with B-ALL may suffer from fulminant clinical course when diagnosed with COVID-19 and could be prone to recurrent SARS-CoV-2 infection. Our experience highlights the importance of optimizing isolation measures and raising awareness for need of blood products to avoid treatment delay. Further research can aid in forming recommendations to prevent management pitfalls especially with the anticipation of a second wave of this pandemic.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal